Confused about building and establishing your milk supply? If you need help or support, or just want to know what to expect, read our guide on breastfeeding in the first month.
The early weeks of breastfeeding are a steep learning curve and if you find it overwhelming from time to time you’re not alone. While feeding around the clock is usual and helps you build your milk supply, it can be tiring. So be patient, look after yourself, and rest assured it will get much easier after this first month as your milk supply becomes established.
How often can I expect to feed?
Your newborn has a small stomach that grows rapidly, from the size of an apricot at week one to the size of a large hen’s egg at two weeks, to perfectly accommodate your growing milk supply.1,2 Allowing your baby to take what she needs, when she needs it, will help her regain her birth weight and continue growing.
“You can expect to feed every two to three hours during the day. At night you might get longer gaps, like three to four hours, or maybe even five,” says Cathy Garbin, an internationally renowned lactation consultant. “But remember each day is different and so is every baby. Some babies are speedy feeders and are full in 15 minutes, whereas others can feed for up to an hour. Don’t compare your feeding pattern to those of others – they’re likely to be completely different.”
At each feed, allow your baby to take as much milk as she wants from one breast, then offer the other, which she may or may not want. When she’s full, she’ll detach naturally and seem relaxed and content – so much so that she might fall asleep. Next time offer the opposite breast first. You can use an app to keep track of which side you’re feeding from.
Why does my baby want to feed all the time?
This first month is usually the most demanding when it comes to breastfeeding. But just because your baby appears constantly hungry and is feeding really often – perhaps every 45 minutes – don’t assume that you don’t have enough milk.
Babies need to feed frequently in order to initiate and build your milk supply during this first month. This lays the foundations of a good milk supply for the future too.3
Don’t forget that babies also want to be in almost constant contact with their mums – the bright lights and sounds of the outside world can seem scary at first and your baby needs your contact to stay calm.
Sara, mum of three, UK, agrees: “Crying isn’t always a sign of hunger – sometimes my babies just wanted to be with me or suck for comfort. Use a sling. Get a bedside crib. Don’t look at the clock. Rest whenever possible. Cleaning does not matter. Make people look after you. Not for three days – at least six weeks! Enjoy the cuddles and cosiness, and never doubt your body.”
Does my baby need a breastfeeding schedule?
Your baby is too young for a routine, so forget following a breastfeeding schedule – let her guide you instead.
“You can read books about how to get a baby on to a schedule, but babies don’t read and don’t understand them,” says Cathy. “Each baby is an individual. Some may conform but many don’t. Most will find their own schedule over time.”
Some mums say a set routine was best for their baby – but these babies were probably among the small percentage who would naturally feed every four hours anyway! Adults generally don’t eat and drink the same things, at the same times, every day, so why should your baby follow such a strict routine?
Instead, offer your baby your breast whenever she shows signs of being hungry. Crying is a late sign, so look out for earlier cues, such as her licking her lips, opening her mouth, sucking her hands, or turning her head open-mouthed – known as ‘rooting’.4
What is a let down?
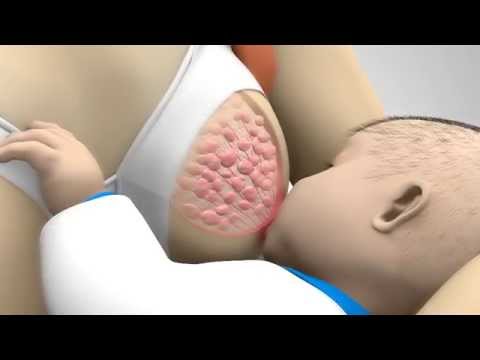
At the start of each feed your hungry baby will suck rapidly on your nipple, prompting the ‘let-down’ reflex that pushes milk through your milk ducts.5
“Nipple stimulation triggers the brain to release the hormone oxytocin,” explains Cathy. “The oxytocin goes through your body and causes the little muscles around the milk-making glands in the breast to contract. It also dilates all the ducts that the milk comes through, so the milk starts to flow.
“If you don’t get a let down, the milk won’t flow freely. It’s a hormonal response and being stressed can stop it happening or working properly. That’s why it’s really important to be supported and comfortable during a feed.
“Research has found that every mum has a pattern of let downs throughout a breastfeed,” she continues. “Oxytocin is a short-acting hormone and might only last in the body for 30 to 40 seconds. Your milk will flow and your baby will drink. Then the oxytocin will dissipate, you’ll get another let down and she’ll feed again, and so on. This is why babies stop and have short rests throughout a breastfeed – it’s nature’s way.”
The let down might cause a strong whooshing or tingling sensation in your breasts, although studies suggest 21% of breastfeeding mums feel nothing,5 as Cathy explains: “Many women will feel the first let down, but not subsequent ones. Don’t worry if you don’t feel a let down – if your baby is feeding well it may be that you simply don’t recognise what it is.”
How do I know if my milk is satisfying my baby?
Because you can’t see how much milk your baby drinks when breastfeeding, you may worry she isn’t getting enough. Try to trust in your body and your baby.
As the milk starts to flow you may notice your baby slows her sucking rhythm. Some mums can clearly hear their baby gulping down the milk, while others may not. Your baby will tell you if she’s had enough, so watch her cues. Many babies may take one, two or three sittings at the breast before they are finished.6
“When your baby gets a good feed she will usually seem ‘milk drunk’ immediately afterwards. She’ll be relaxed and her body language will show you she’s satiated,” says Cathy. “Remember her nappies are also a good indicator that she is getting enough milk. At this stage, your breastfed baby will have five or more wet nappies a day and at least two soft, yellow poos – usually more.”
From one month onwards your exclusively breastfed baby’s poo should look the same every day (yellow, seedy in texture, loose and watery) until you start to introduce solids from around six months. Your baby may poo daily, or only poo every two to three days, or even less frequently than that.7
When should my baby regain her birth weight?
Most newborns will lose weight during the first few days after birth. This is normal and nothing to worry about. Most lose around 5 to 7% of their birth weight, but some may lose up to 10%. However, nearly all babies are back up to birth weight by day 10 to 14. In the first three to four months the minimum expected weight gain is 150 g (5.5 oz) per week on average. But remember babies can have really fast weeks of growth, as well as slower ones, so your healthcare professional will be looking at your baby’s overall wellbeing and growth continuously.7,8
If you’re concerned – or your baby shows signs of dehydration, such as dark-coloured urine, no poos for more than 24 hours, a sunken fontanelle (the soft spot on her head), jaundice, lethargy, floppiness, and not wanting to feed (i.e. going four to six hours without a feed) – seek medical advice quickly.7
What is cluster feeding?
When a baby wants to breastfeed very frequently over the space of several hours, this is known as cluster feeding.6 It often peaks in the evenings between 18:00 and 22:00, which coincides with when many babies are unsettled and want to be held a lot. Mums most often report this happening during two to nine weeks after birth. This is a very normal, common behaviour for babies who are otherwise content during the rest of the day, feeding and gaining weight well, and generally healthy.9
Your baby may be cluster feeding because she’s having a developmental spurt and needs to feel secure, reassured and loved. She may be finding it hard to switch off due to all the stimulation her growing brain is receiving, or she may simply feel overwhelmed by it.9 Young babies who are overtired can find it hard to calm themselves and need someone to help. And what better way to be calmed than having a breastfeed, which is not just a source of food, but also a pain reliever and happy hormone giver?10
“No one had spoken to me about cluster feeding, and 10 days in I was beside myself, convinced my milk supply wasn’t meeting my baby’s needs,” remembers Camilla, mum of one, Australia. “It was a confusing time. I was told to pump and ‘top up’, until I called the Australian Breastfeeding Association. They explained what was going on and that it wasn’t a supply issue.”
Remember this is a temporary phase. Try preparing your evening meal at a time in the day when your baby is sleeping well, so you can just reheat it and eat quickly during the cluster feeding period. If you have support, share holding and rocking your baby to give you a break. If you don’t have support and feel it’s all too much and you’re not coping, place your baby safely in her cot and calm down for a few minutes before coming back to hold her again.
Enlist your partner, family and friends to help with chores, meals and any older children. If you have the resources, you could consider paying someone to help around the home. Try to have plenty of rest, eat well and stay hydrated.
“My daughter would sleep a lot during the day and then want to cluster feed from about 23:00 to 05:00, which was exhausting,” says Janelle, mum of one, US. “My husband tried to lighten the burden wherever he could: cleaning, making food for me, doing laundry, changing diapers, letting me sleep whenever possible, and always reassuring me that we were doing the best we could.”
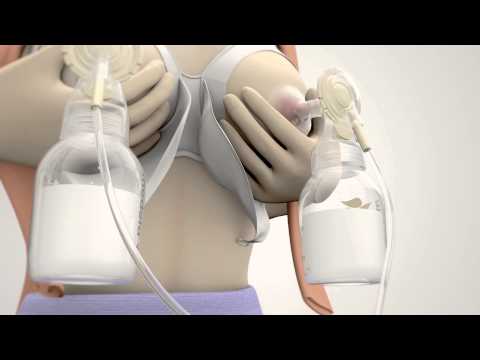
If you’re concerned about the intensity of breastfeeding, it’s worth seeking help. “You need to see a lactation consultant or breastfeeding specialist, to find out if there’s an underlying problem,” explains Cathy. “Don’t fall into the trap of topping up with formula (unless advised to by your healthcare professional) until you get to the root cause. It could be that you’re not producing enough milk, but it might be that your baby is not able to get the milk effectively.”
When will breastfeeding get easier?
This early phase is short and special, and although it sometimes feels relentless it will get easier! By the end of one month, your breast milk supply will be established, and your baby should be stronger and more effective at feeding.2,3 Any issues with your baby’s latch are likely to be sorted, and your body will be more efficient at making milk, so any soreness or leaking should start to subside.
“The first four to six weeks are the toughest, then it starts to settle down,” says Cathy. “And when you get to three months, breastfeeding gets really easy – way easier than cleaning and making up a bottle. Just hang in there!”
And the longer you continue breastfeeding, the more you’ll enjoy the benefits – from saving money on formula and having better sleep,11–13 to boosted immunity for your baby14 and enhanced protection against certain cancers for you.15
“When you think you can’t go on, take it feed by feed and day by day,” advises Hannah, mum of one, UK. “I was sure I’d never make it to eight weeks. Now it’s almost 17 weeks and (dare I say it) easy.”
Find out about the next step on your breastfeeding journey in Breastfeeding after a month: What to expect
- Naveed M et al. An autopsy study of relationship between perinatal stomach capacity and birth weight. Indian J Gastroenterol.1992;11(4):156-158.
- Neville MC et al. Studies in human lactation: milk volumes in lactating women during the onset of lactation and full lactation. Am J Clinl Nutr. 1988;48(6):1375-1386.
- Kent JC et al. Principles for maintaining or increasing breast milk production. J Obstet, Gynecol, & Neonatal Nurs. 2012;41(1):114-121.
- Australian Breastfeeding Association [Internet]. Feeding cues; 2017 Sep [cited 2018 Feb].
- Kent JC et al. Response of breasts to different stimulation patterns of an electric breast pump. J Human Lact. 2003;19(2):179-186.
- Kent JC et al. Volume and frequency of breastfeedings and fat content of breast milk throughout the day. Pediatrics. 2006;117(3):e387-395.
- Lawrence RA, Lawrence RM. Breastfeeding: A guide for the medical profession; 2011. 1114 p.
- World Health Organisation. [Internet]. Child growth standards; 2018 [cited 2018 Feb]
- Australian Breastfeeding Association. [Internet]. Cluster feeding and fussing babies; Dec 2017 [cited 2018 Feb]
- Moberg KU, Prime DK. Oxytocin effects in mothers and infants during breastfeeding. Infant. 2013;9(6):201-206.
- U.S. Department of Health & Human Services [Internet]. Surgeon General Breastfeeding factsheet; 2011 Jan 20 [cited 2017 Feb]
- Kendall-Tackett K et al. The effect of feeding method on sleep duration, maternal well-being, and postpartum depression. Clinical Lactation. 2011;1;2(2):22-26.
- Brown A, Harries V. Infant sleep and night feeding patterns during later infancy: Association with breastfeeding frequency, daytime complementary food intake, and infant weight. Breast Med. 2015;10(5):246-252.
- Hassiotou F et al. Maternal and infant infections stimulate a rapid leukocyte response in breastmilk. Clin Transl immunology. 2013;2(4).
- Li DP et al. Breastfeeding and ovarian cancer risk: a systematic review and meta-analysis of 40 epidemiological studies. Asian Pac J Cancer Prev. 2014;15(12):4829-4837.